Prostate biopsy
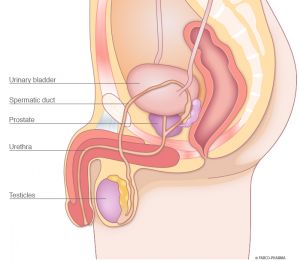
The prostate, a gland that produces seminal fluid
The prostate is an exocrine gland below the urinary bladder that encircles the male urethra. It is a firm, partially glandular/partially muscular mass approximately the size of a chestnut and weighs about 10 - 20 g. The prostate produces the majority of seminal fluid and many of the enzymes it contains. The sperm, which originate in the testicles, are mixed with the seminal fluid here and activated.
Factors that justify a prostate biopsy
If the presence of a prostate disease is suspected or in the case of abnormal findings within the scope of an early detection examination, a prostate biopsy (also called a prostate punch biopsy) may be necessary in order to confirm or rule out the diagnosis.
Early detection is especially important in the case of prostate cancer because this type of cancer rarely causes symptoms in the early stage. At the same time, the earlier treatment can begin, the better the prospects for a complete recovery.
Suspicious or unclear findings may include one or more palpable nodules in the prostate or an elevated PSA value (PSA = prostate-specific antigen). PSA is a protein that is produced exclusively by the prostate and liquefies the seminal fluid. The PSA value is considered to be a prostate-specific tumour marker and denotes the amount of PSA that is circulating in the blood. However, an elevated PSA value may also indicate a benign enlargement of the prostate (prostatic hyperplasia) or an inflammation of the prostate (prostatitis).
Prostate biopsy preparation and implementation
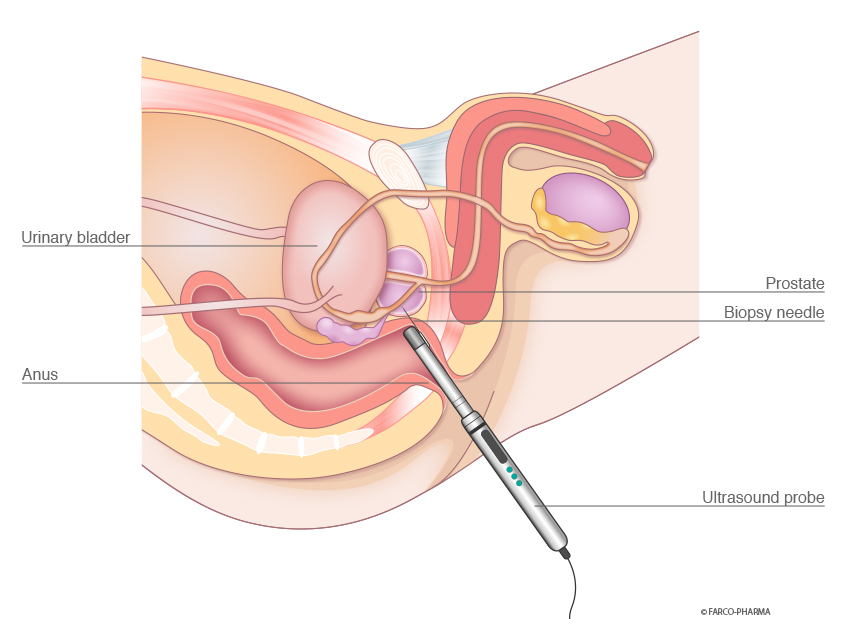
During a prostate biopsy, the patient lies on his side or back with the legs raised and bent. If necessary, the patient may receive a sedative or painkiller prior to the examination.
Prostate biopsies are performed via the anus. The mucosa is locally anaesthetised and lubricated in advance with a sterile lubricant with local anaesthetic and disinfecting properties, such as Instillagel®.
The biopsy is then performed with the aid of transrectal ultrasound (TRUS). Here, a puncture cannula secured to the ultrasound probe is used to collect targeted samples from the prostate. Multiple, small, cylindrical samples approx. 15 mm in length are punched out of the prostate. Characteristics, such as size, abnormalities and shape are readily able to be assessed using this type of sample collection.
A total of about 10 - 12 punch biopsies are usually collected. This is necessary in order to identify the severity and extent of any potential prostate cancer and to define the subsequent treatment.
The punch biopsies are collected with the biopsy device and the process is barely noticeable. As a precaution, the treating physician commonly prescribes an antibiotic in order to prevent an infection following the prostate biopsy.
Procedure following the prostate biopsy
Nowadays, prostate biopsies are usually performed as an outpatient procedure in hospital or at private urology practices. Hospitalisation and general anaesthetic are only necessary in rare cases.
The procedure itself lasts only a few minutes; however, patients still remain in hospital or at the medical practice for a while under observation. Before the patient is released to go home, a urine test is performed to ensure that there is no heavy bleeding.
Following biopsies, patients should rest for one to two days. Patients may experience a minor pressure sensation and a painkiller may be necessary in some cases. A little blood in the stool, urine or sperm is common following biopsies and clears up on its own after a few days.
Potential complications following prostate biopsies
Circulatory problems may occur immediately during or after a prostate biopsy. These issues are usually able to be brought under control quickly by administering fluids and raising the patients legs.
In the case of heavy bleeding, fever over 38.0°C, difficulty urinating or testicular pain, you should contact your physician immediately.
Prostate biopsy results
The tissue samples are examined by a pathologist under a microscope. The type and malignancy are determined in the case of pathological changes (positive biopsy).
If there is no pathological tissue (negative biopsy), then this may mean that there is actually no cancer present or that the tissue was not collected properly.
If cancer continues to be suspected, e.g. due to palpable nodules in the prostate or an elevated PSA value, then it may be necessary to perform another biopsy following a certain period.
Your physician will explain your findings to you and discuss how to proceed.